SK. 11 Early Warning Signs Your Body Might Be Headed Toward Diabetes
Disclaimer: This content is for informational purposes only and should not be considered a substitute for professional medical advice. Always consult your doctor if you experience any concerning symptoms.

Diabetes often develops silently, with early symptoms that are easy to miss. Prediabetes—when blood sugar levels are higher than normal but not yet in the diabetes range—is your body’s early warning sign. Recognizing the signs can help you take steps to prevent type 2 diabetes before it becomes a more serious condition.
In this article, we’ll highlight 11 subtle changes your body may show that shouldn’t be ignored.
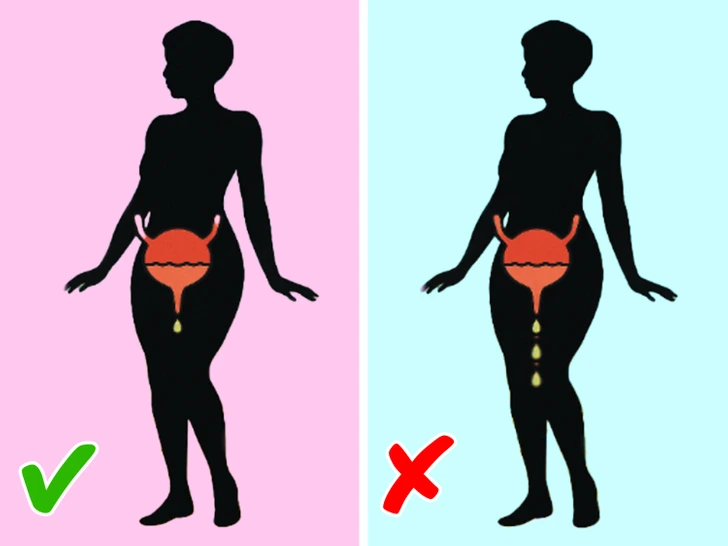
1. Persistent Thirst and Frequent Urination
Feeling unusually thirsty or needing to urinate more often can be early signs of high blood sugar. When glucose builds up in the bloodstream, the kidneys work harder to remove the excess, leading to dehydration and increased thirst. This cycle can cause you to drink more and urinate more frequently than usual.
2. Blurred Vision

Sudden changes in vision—especially blurry eyesight—can be a signal of fluctuating blood sugar levels. High glucose levels can cause swelling in the eye lens, affecting your ability to focus. While vision may return to normal with proper treatment, chronic high blood sugar can lead to lasting eye issues if left unchecked.
3. Unusual Fatigue

Feeling tired all the time, despite getting enough sleep, can stem from the body’s inability to use glucose efficiently. When cells don’t receive the energy they need, fatigue can set in. Dehydration from frequent urination can also contribute to this sense of constant exhaustion.
4. Tingling or Numbness in Hands and Feet

Tingling, numbness, or burning sensations in the extremities may indicate nerve damage caused by elevated blood sugar. Known as peripheral neuropathy, this condition is common in people with prediabetes or diabetes and typically starts in the hands or feet.
5. Slow Healing of Cuts and Wounds
When wounds take longer than usual to heal, it could be due to impaired blood circulation and inflammation caused by high glucose levels. This issue is especially concerning in the feet, where unnoticed sores can lead to more serious complications.
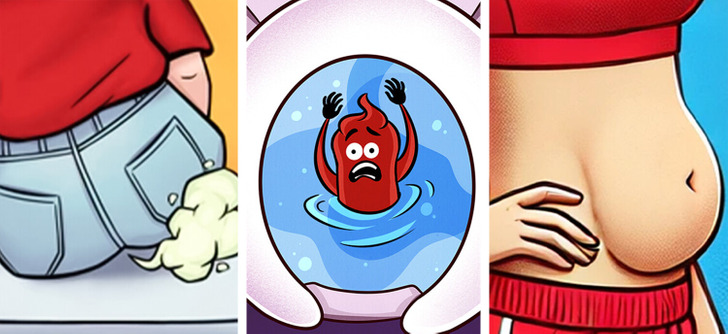
6. Increased Hunger Even After Meals

Are you constantly hungry—even after eating a full meal? If so, it might be because your body isn’t processing glucose effectively. Insulin resistance can prevent cells from getting the fuel they need, leading to persistent feelings of hunger.
7. Digestive Discomfort: Bloating, Constipation, and Gas
Blood sugar imbalances can affect gut function. High glucose levels may interfere with the nerves that control digestion, slowing down bowel movements and leading to symptoms like constipation, bloating, or excess gas. If digestive issues are ongoing, they could be related to glucose regulation.
8. Dry Mouth and Bad Breath

Reduced saliva production, often linked to high blood sugar, can cause a dry mouth and unpleasant breath. Dry conditions in the mouth allow bacteria to thrive, increasing the risk of gum disease and other oral health issues.
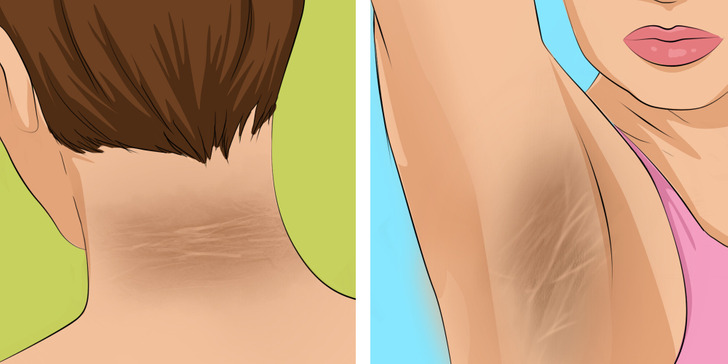
9. Skin Changes: Itching, Discoloration, or Rashes

Dry, itchy skin or unusual darkened patches—especially in areas like the neck, underarms, or groin—may be signs of insulin resistance. A condition called acanthosis nigricans can cause these dark, velvety patches, often signaling a higher risk for developing diabetes.
10. Mood Changes, Headaches, and Brain Fog

Frequent mood swings, irritability, or headaches may result from fluctuating blood sugar levels. Many people also report difficulty concentrating or experiencing mental “fogginess.” Since the brain depends on a steady supply of glucose to function properly, imbalances can affect mental clarity and emotional stability.
11. Recurring Infections, Especially Yeast Infections
High blood sugar can create an environment where yeast and bacteria thrive, leading to more frequent infections. These may appear in moist areas of the body, such as the mouth, skin folds, or other sensitive areas. Recurring infections should always be checked by a medical professional.
What You Can Do to Lower Your Risk
The good news is that prediabetes is reversible with lifestyle changes. Early intervention can significantly reduce the risk of progressing to type 2 diabetes. Here are some evidence-based tips:
1. Maintain a Balanced Diet
Focus on whole foods such as vegetables, fruits, lean proteins, and whole grains. Limit processed foods, added sugars, and saturated fats.
2. Get Regular Physical Activity
Aim for 30–60 minutes of moderate exercise—like brisk walking, cycling, or swimming—on most days of the week. Exercise helps your body use insulin more efficiently.
3. Manage Your Weight
Losing even 5–10% of your body weight can improve insulin sensitivity and lower blood sugar levels.
4. Stay Hydrated
Choose water over sugary beverages. Hydration supports kidney function and helps regulate blood sugar.
5. Prioritize Sleep
Poor sleep quality has been linked to insulin resistance. Aim for 7–9 hours of quality sleep each night.
6. Monitor Your Health
Routine health screenings, including blood glucose tests, are essential—especially if you have risk factors like a family history of diabetes, obesity, or high blood pressure.
7. Seek Professional Help
A registered dietitian or certified diabetes educator can help tailor a lifestyle plan to your needs. In some cases, your doctor may recommend medication such as metformin to help manage blood sugar.
Final Thoughts
Prediabetes often develops quietly, but your body might already be signaling that something’s off. Paying attention to early symptoms and making healthy changes can make all the difference. If you recognize several of these signs, consult a healthcare professional for further evaluation.
Remember: Awareness and action are the most powerful tools in preventing diabetes.