HT6. Poop and Colon Cancer: Early Warning Signs and When to Seek Help
Many people assume that only major symptoms indicate serious health issues, but subtle changes in stool can serve as early warning signs of colon cancer. Symptoms such as blood in stool, changes in consistency, and alterations in bowel movement frequency can sometimes point to underlying health concerns. While these signs are not always indicative of colon cancer—since other digestive disorders can present similarly—it’s important to recognize them and know when to seek medical attention.
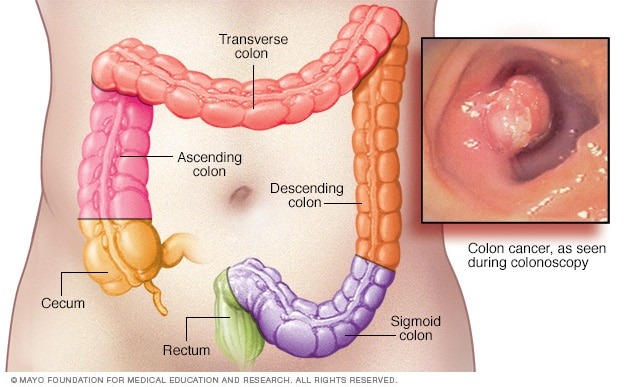
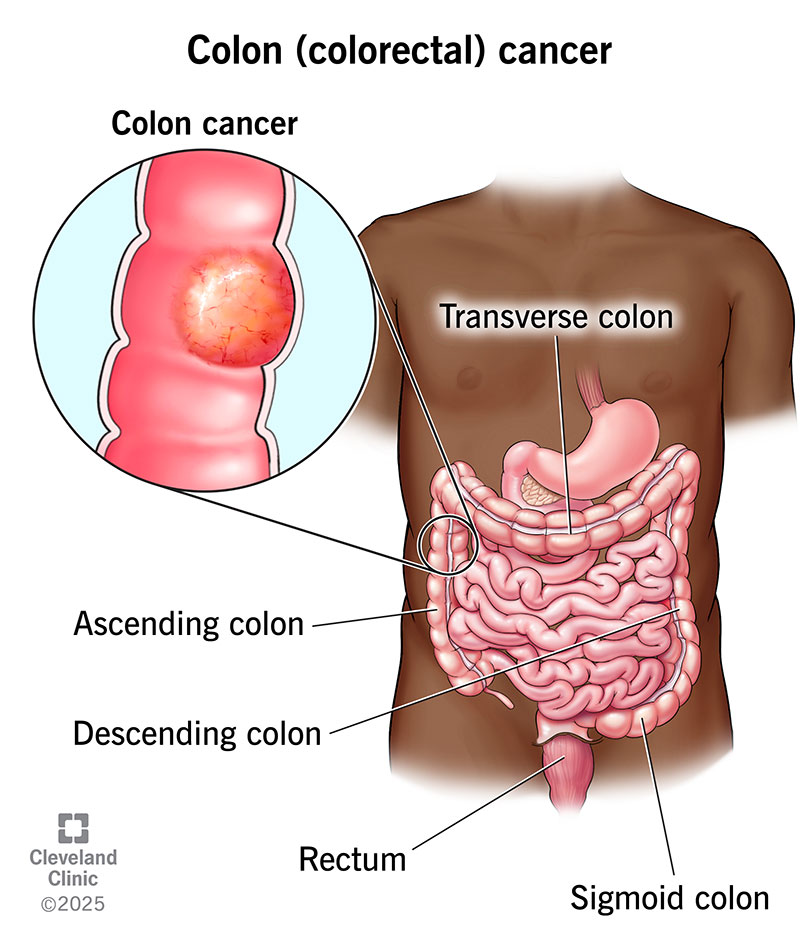
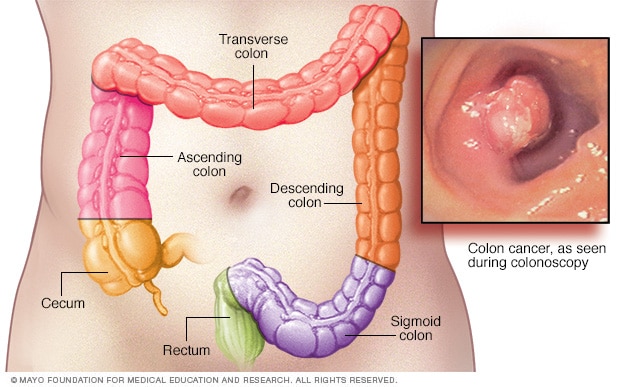
Understanding Colon Cancer
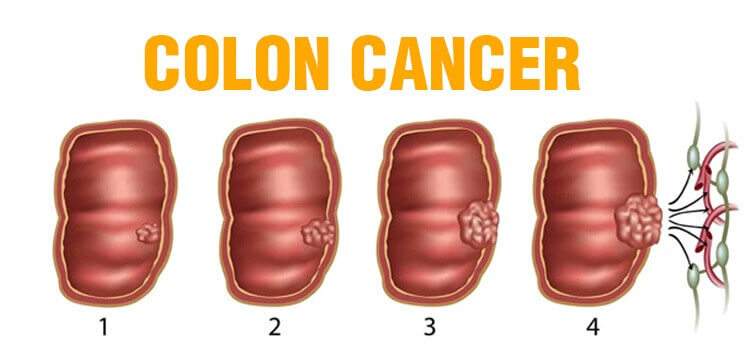
Colon cancer, also known as colorectal cancer, develops in the colon or rectum and is one of the most common types of cancer worldwide. It often begins as benign growths called polyps, which can evolve into cancerous tumors over time. The progression from polyps to cancer can take years, making early detection crucial for successful treatment.
The primary risk factors for colon cancer include:
- Age (risk increases with age, particularly after 50)
- Family history of colorectal cancer
- Diet high in red and processed meats
- Sedentary lifestyle
- Obesity
- Smoking and excessive alcohol consumption
- Chronic inflammatory conditions such as Crohn’s disease or ulcerative colitis
Understanding these risk factors, combined with awareness of potential symptoms, can help individuals take proactive steps to monitor their health.
Colon Cancer and Poop: Early Indicators

One of the first signs that something may be wrong is a disruption in normal bowel habits. Certain stool changes, such as narrowing, discoloration, or an ongoing sensation of incomplete evacuation, could be indicators of colon cancer:
- Narrow “pencil” stools – A tumor in the intestinal passage may cause stools to become thinner.
- Painful bowel movements (dyschezia) – Often associated with rectal cancer.
- Persistent feeling of incomplete evacuation (tenesmus) – A potential early-stage rectal cancer symptom.
- Rectal bleeding – A common sign, especially with tumors in the lower bowel.
- Abdominal pain – Can be triggered by inflammation affecting pain receptors.
- Unexplained fatigue – Often linked to anemia resulting from internal blood loss.
Poop Changes in Regional Colon Cancer
By the time colon cancer reaches stage three, it may have spread to nearby lymph nodes. This can lead to more pronounced bowel changes as tumors penetrate deeper into intestinal tissue:
- Constipation – Tumor-related blockages may slow digestion.
- Diarrhea – Fluids bypassing partial blockages can cause loose stools.
- Alternating constipation and diarrhea – This irregular pattern could signal serious concerns.
- Blood in stool (hematochezia) – May vary in color depending on the tumor’s location.
- Worsening tenesmus – Caused by growing tumors and increasing inflammation.
- Bloating and abdominal cramps – Gas build-up may occur due to narrowed bowels.
- Iron-deficiency anemia symptoms – Nearly half of individuals with colon cancer experience anemia.
Scar tissue and strictures can develop as tumors grow, occasionally leading to complete or partial bowel obstructions. Even if blood is not visible in stool, internal bleeding may still be occurring.
Poop Changes in Advanced Colon Cancer
At stage four, colon cancer typically spreads to distant organs. Obstruction and bleeding become more severe, making symptoms increasingly noticeable. If the tumor is located on the right side of the colon, stools may appear dark and sticky (melena) due to the mixing of blood, oxygen, and hemoglobin during digestion.
- Nausea and vomiting – Common as blockages worsen.
- Unexplained weight loss – Chronic inflammation can suppress appetite, leading to muscle loss.
At this advanced stage, bowel wall integrity may weaken, increasing the risk of perforations. If cancer has spread to the liver, lungs, or bones, additional symptoms may appear. However, some individuals with stage four colon cancer may not experience significant bowel-related symptoms if blockages or bleeding are not present.
Diagnosis and Screening for Colon Cancer
Early diagnosis of colon cancer dramatically improves the chances of successful treatment. Common diagnostic methods include:
- Colonoscopy – A procedure that allows doctors to examine the entire colon and remove polyps if necessary.
- Fecal Occult Blood Test (FOBT) – A test that detects hidden blood in stool samples.
- Stool DNA Test – A newer test that looks for specific DNA changes associated with colorectal cancer.
- CT Colonography (Virtual Colonoscopy) – A less invasive imaging test.
- Blood Tests – Used to check for anemia, liver function, and other markers that may indicate cancer.
Regular screenings are recommended for individuals over 50, though earlier screenings may be advised for those with a family history of colorectal cancer or other risk factors.
Preventing Colon Cancer
While some risk factors, such as age and genetics, cannot be changed, lifestyle modifications can significantly reduce the risk of developing colon cancer:
- Adopt a fiber-rich diet – Increase intake of fruits, vegetables, and whole grains.
- Limit red and processed meats – Studies suggest these foods may contribute to an increased cancer risk.
- Exercise regularly – Physical activity helps maintain a healthy digestive system and lowers cancer risk.
- Maintain a healthy weight – Obesity has been linked to a higher risk of colon cancer.
- Avoid smoking and limit alcohol consumption – Both are associated with an increased risk of colorectal cancer.
- Stay hydrated – Drinking plenty of water promotes regular bowel movements and a healthy colon.
When to See a Doctor
It’s important to consult a healthcare professional if any of the following symptoms persist for more than a few weeks:
- Persistent changes in bowel habits (diarrhea, constipation, narrowing of stool)
- Rectal bleeding or blood in stool
- Persistent abdominal discomfort, cramps, or bloating
- Unexplained weight loss
- Weakness or fatigue
While these symptoms do not necessarily indicate colon cancer, they warrant further investigation to rule out serious conditions.
Key Takeaways
Understanding the link between poop and colon cancer is crucial, as seemingly minor changes in bathroom habits could serve as early red flags. Persistent blood in the stool, narrowing of stools, frequent diarrhea, or increased bowel movements can indicate underlying issues. However, other gastrointestinal conditions can mimic these symptoms, so it’s essential not to jump to conclusions.
If you notice unusual or persistent changes in your bowel movements, consult a healthcare provider. Early detection significantly improves the prognosis for colon cancer, making timely medical evaluation vital.
Please SHARE this article with your friends and family on Facebook to raise awareness.