SK. Study Suggests Key Link That Could Help Explain Autism Development
Recent research has drawn significant attention to the growing understanding of how our gut microbiota influences not only physical health but mental health and neurological development as well. Over the years, studies have increasingly highlighted the connection between gut health and various conditions, ranging from mental health issues and autoimmune diseases to neurological disorders like autism.
One of the latest breakthroughs comes from a study published in The Journal of Immunology, which suggests a key link between gut microbiota and autism. But what’s even more fascinating is that the study proposes that our mother’s microbiota—rather than our own—might play a more crucial role in shaping our likelihood of developing autism.
The Role of the Gut Microbiota
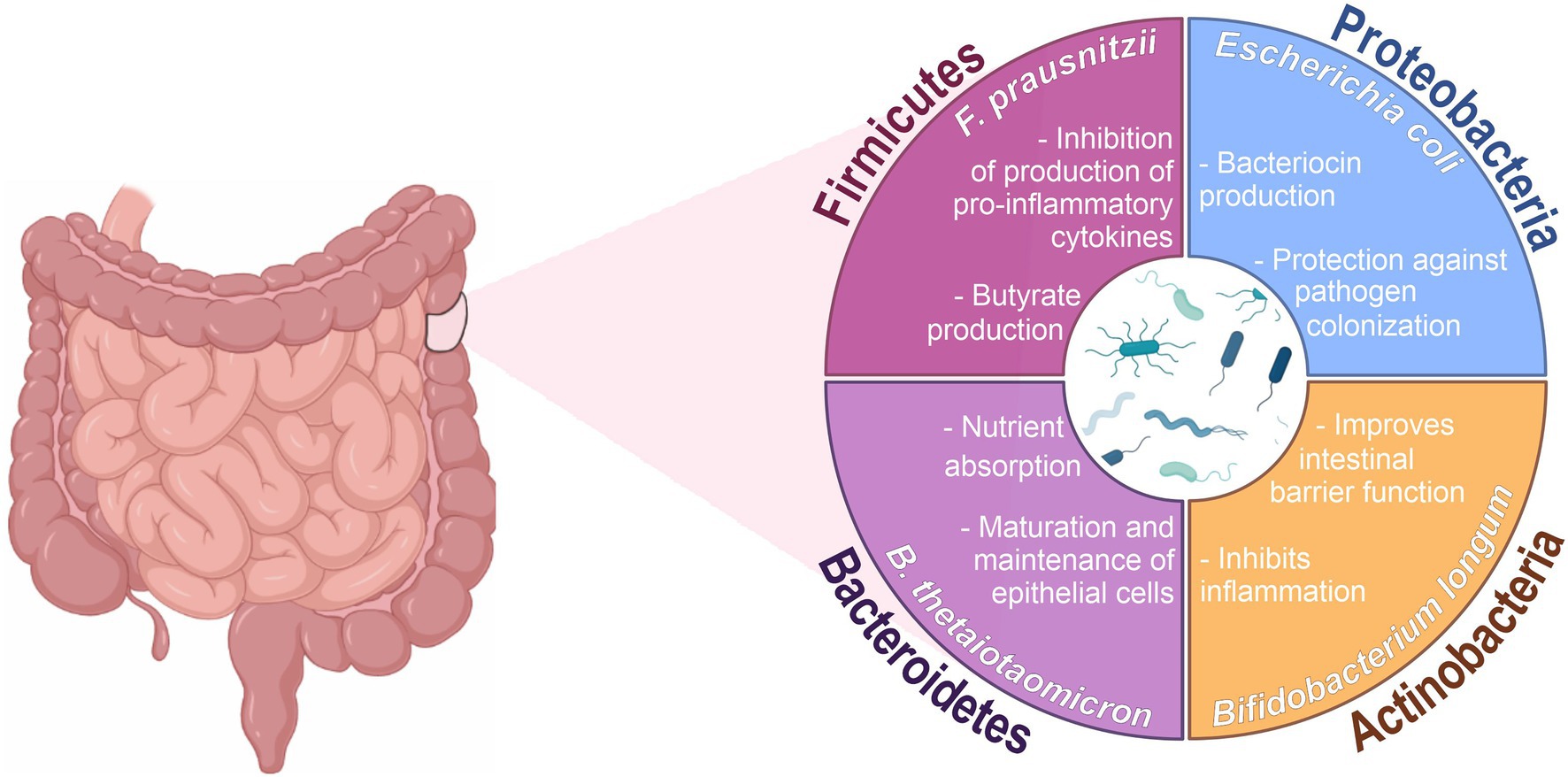
The gut microbiota is the collection of microorganisms living in our digestive system, and it has a significant influence on our overall health. These microorganisms interact with various systems in the body, including the immune system and the brain. Researchers have found that the microbiota can affect everything from immune responses to mental health, stress reactions, and even our body’s ability to fight off infections.
But as new research shows, the microbiota’s impact extends beyond just general health. A study by John Lukens, a PhD student at the University of Virginia School of Medicine, and his team, reveals a fascinating connection between gut microbiota and the neurodevelopmental disorder autism. According to Lukens, the microbiome plays a critical role in shaping how the developing brain responds to environmental influences, especially stress, infection, and injury. This could have profound implications for understanding the development of autism.
Gut Microbiota and Autism: A Closer Look
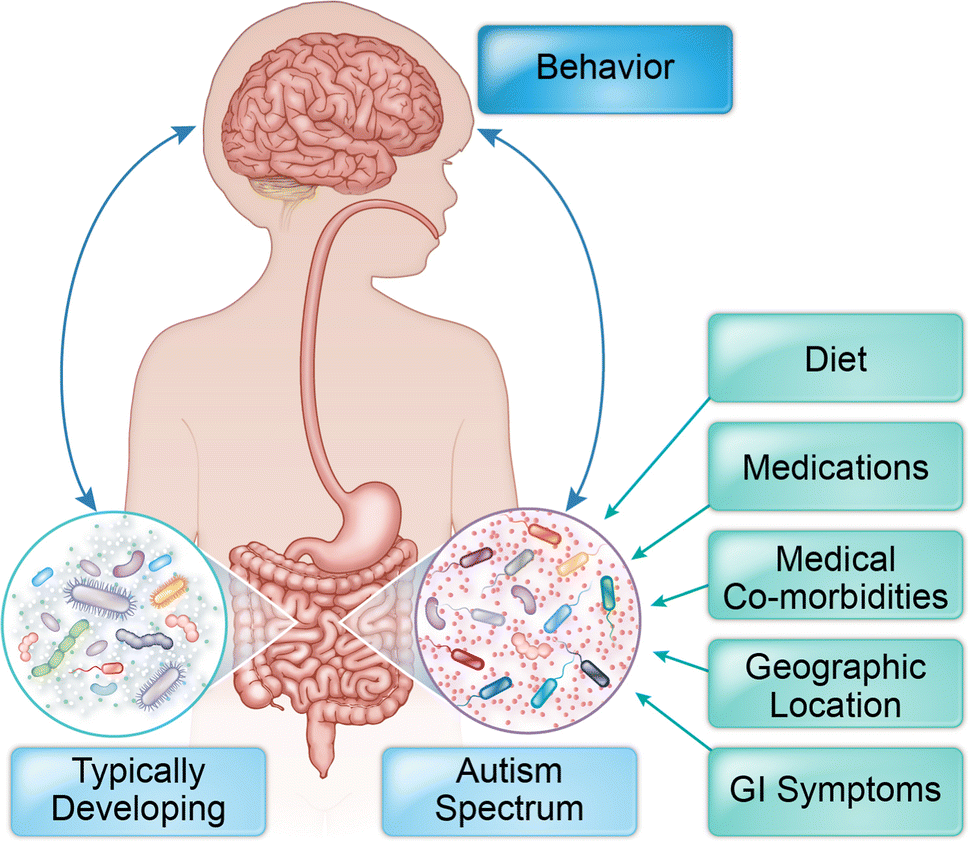
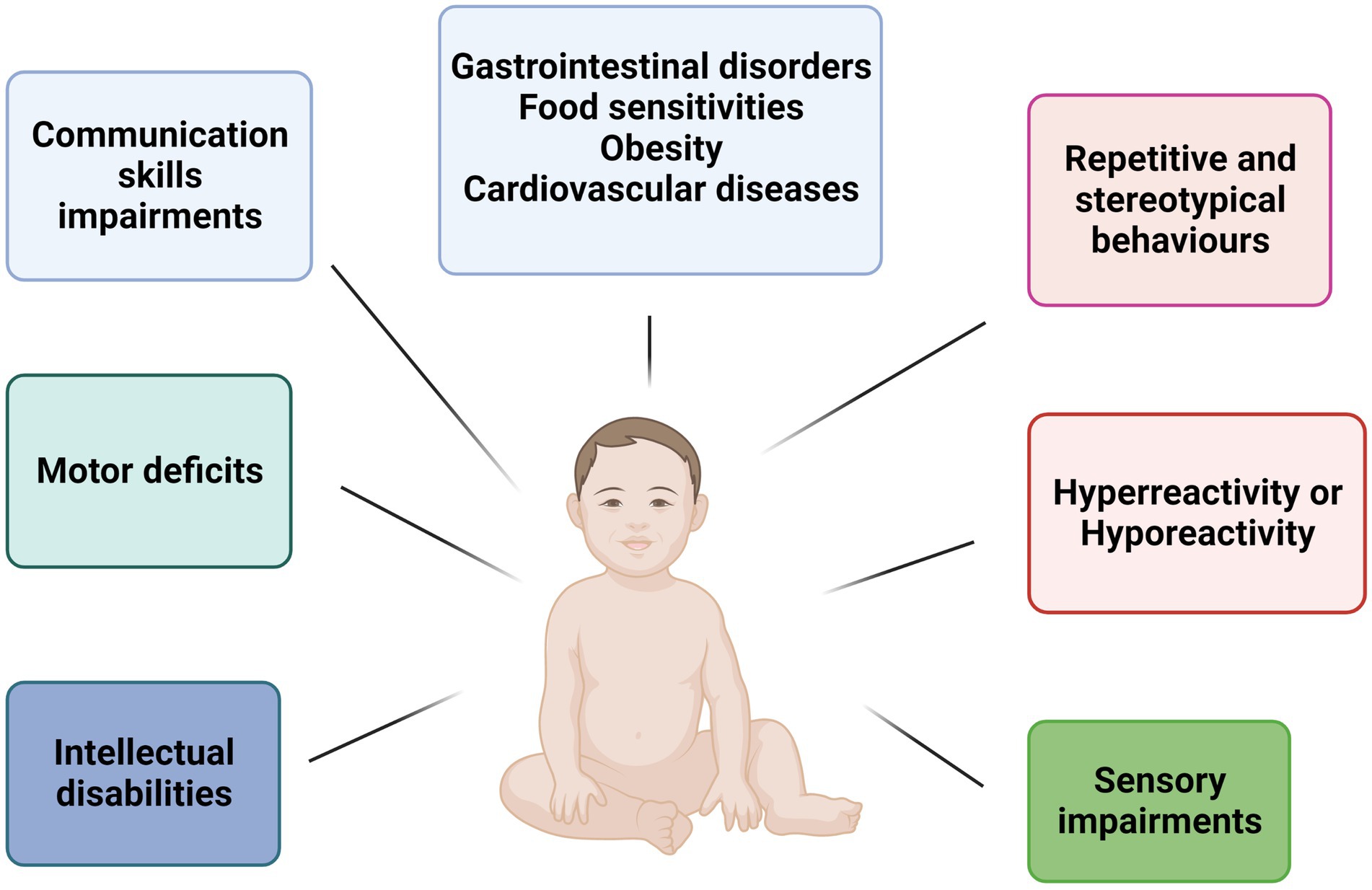
In the study, the team used animal models to explore how microbiota might affect brain development, specifically in relation to autism. Autism, a neurodevelopmental disorder, is characterized by challenges with social interactions, communication, and repetitive behaviors. While the exact cause of autism is still unclear, researchers have long suspected a connection to environmental and immune system factors during pregnancy.
Lukens and his team focused on a specific molecule known as interleukin-17a (IL-17a), which plays a crucial role in the body’s immune response. IL-17a is already associated with conditions such as psoriasis, multiple sclerosis, and rheumatoid arthritis. It’s also instrumental in protecting the body from infections, particularly fungal infections. However, IL-17a’s role is not just limited to immune defense—it can also influence brain development in the fetus while still in the womb.
The researchers hypothesized that a disruption in the immune system, driven by the microbiota, could affect IL-17a production, which in turn may contribute to neurodevelopmental disorders like autism.
How the Study Was Conducted

To test their theory, the research team used laboratory mice, specifically female mice from two different labs, to examine how microbiota affects brain development and immune responses. The mice from the first lab had gut microbiota that predisposed them to an inflammatory response triggered by IL-17a. In contrast, the mice from the second lab had a normal microbiota, serving as a control group.
The experiment involved suppressing IL-17a in both groups of mice to see how it affected their neurodevelopment. After suppressing IL-17a, the pups from both groups exhibited normal, neuro-typical behaviors at birth. However, when everything was allowed to grow without further interference, the pups born to mothers in the first group—those with microbiota predisposed to inflammation—developed a neurological disorder resembling autism. The condition affected their social behaviors and led to repetitive actions, both hallmark symptoms of autism.
Fecal Transplants Confirm the Link
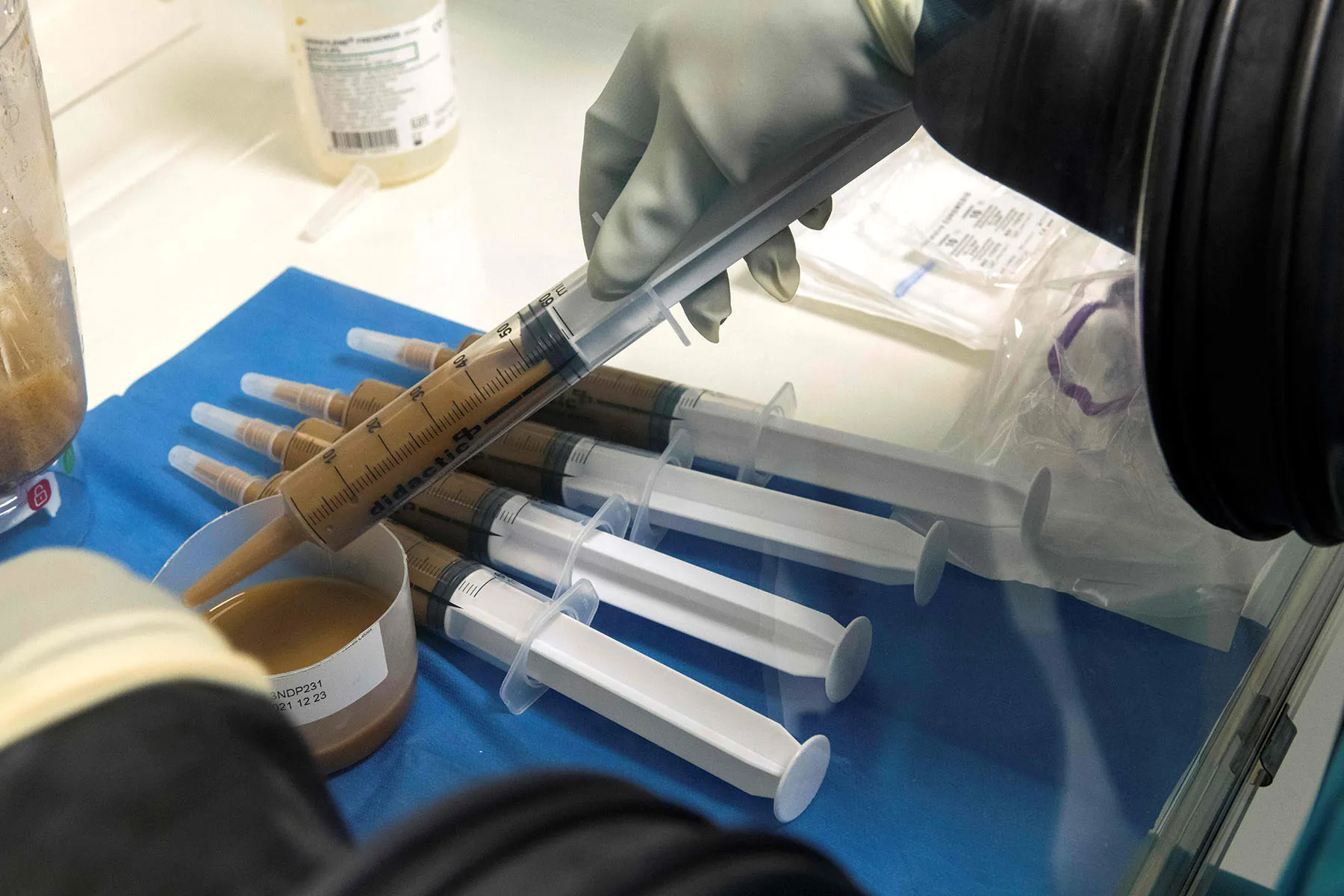
To further investigate, the researchers performed a fecal transplant from the first group of mice (those with the inflammatory microbiota) to the second group. The goal was to alter the second group’s microbiota to more closely resemble that of the first. The results were striking: just like the pups in the first group, the second group’s pups began to develop similar neurological disorders resembling autism.
This discovery is groundbreaking because it suggests that the mother’s microbiota, rather than the offspring’s, might play a significant role in influencing the development of neurodevelopmental disorders. Though these findings are still based on animal models and further research is needed, they provide compelling evidence that the health of the mother’s gut microbiota during pregnancy could impact the likelihood of autism development in her children.
Implications for Human Autism Research
While the study is still in its early stages, it raises important questions about how environmental factors, particularly the mother’s gut health, influence the development of autism. According to Lukens, the next step is to identify the specific components of the mother’s microbiome that are linked to autism development and to see if similar correlations can be found in humans.
As of now, IL-17a is just one molecule in a much larger picture. Lukens suggests that IL-17a may be just one of many factors influencing autism development and that there are likely other molecules and microbiota interactions at play.
The findings could eventually lead to new preventative measures or therapies, focusing on improving maternal gut health during pregnancy. It might also provide insights into potential treatments for autism, aimed at addressing the immune system or gut microbiota imbalances.
Looking Ahead: What’s Next for Autism Research?
This research opens up new avenues for studying the causes of autism and potentially preventing it. If the theory holds true in human studies, it could revolutionize how we think about prenatal care and the environmental factors that shape brain development. Gut health, often overlooked, could become a critical area of focus for those seeking to reduce the risk of neurodevelopmental disorders.
Researchers are still in the early stages of exploring how these findings apply to humans, and the next step is to identify specific markers within the mother’s microbiota that might influence the developing brain. If scientists can pinpoint what exactly in the microbiome triggers the development of autism, it could lead to targeted interventions that help reduce the risk or severity of the disorder.
Additionally, the broader implications for understanding the role of gut health in mental health and neurological development cannot be overstated. Just as the study has explored the link between gut microbiota and autism, similar research could be done to investigate other neurodevelopmental disorders, potentially offering new solutions and treatments for a variety of conditions.
Conclusion: A Breakthrough in Autism Research
While the link between gut microbiota and autism remains to be fully understood, the research presented by John Lukens and his team is an exciting step forward. It suggests that the health of the mother’s gut during pregnancy may play a significant role in shaping the child’s risk for developing autism. The potential for new, targeted interventions based on this research could offer fresh hope for families affected by autism and other neurodevelopmental disorders.
As scientists continue to explore the complex relationship between the gut and the brain, we may uncover more about how environmental and immune system factors influence brain development. These findings hold promise for advancing our understanding of autism and could lead to breakthroughs in both prevention and treatment.